5 Steps to Making the First Months Easier
So your child will be OK, it’s is time to get into action mode. There are a number of key things that you can do so that your first weeks and months go more smoothly and will help you feel less overwhelmed. Even if you have already been at it for awhile, these steps will be worth reviewing again to make sure that you are making your day to day run as smoothly as possible.
Step 1: Get Organized
My mother in law has a term that she uses for areas that are dedicated to certain of her activities in her house; she calls them “centers.” A term has never been more appropriate for getting organized when it comes to being able to manage your child’s diabetes. You need a “Diabetes Center” in your house or apartment. Whether it is a dedicated cabinet, area in your pantry or wherever it makes sense to you, this will be storage central for the shopping bag of supplies that you pick up from the pharmacy. This will allow you to see what you have or more importantly, what you don’t have or what you are running low on. Once you have everything organized, make sure you have at least two sets of things, including glucose monitors, pens, lancets, a hefty supply of alcohol pads (you will go through them like popcorn) etc. We put a travel bag together as well, that had an emergency glucose kit in it, a travel glucose monitor, swabs, etc. We also got a small copy of the Calorie King book which is good to have along on the road.
We also downloaded the Calorie King app that can be very useful in figuring out carbs on the road and at restaurants. Click on the logo for a link to their site. The other essential tool is a digital scale. We didn’t have one at first, and once we got one, it made our lives much easier, so go ahead and get one right at the beginning. More on this later.
Step 2: Break Down the Carbohydrate Math
One of the early things that we did that proved to be an ultimate lifesaver was we basically went through our kitchen and pulled out everything that our boy eats (the good news is that for kids, the list is actually pretty limited). We then converted the listed “Serving Size” into information on carborhydrate content in each food that was useful to us on a daily basis. An example is, a serving size of Milano Cookies by Peppridge Farm is 3 cookies. That information is essentially useless alone because I guarantee you that your kid will want one or  four cookies, and never a number that is divisible by three. If the Serving Size was two, he will then of course, want three. Given that, it is important to have a list of how many carbs is in one cookie. We set up an excel spreadsheet that we keep on a laptop in our kitchen. We have a tab for every meal that has all the things listed that he typically eats, and how many carbs are in the easily definable quantity that makes sense to use on a daily basis. We use weight for things like fruit and other things that are easily weighed, cookies and easily countable items, we keep on a per item basis. We then set it up so that all we have to do is enter the number of units or the weight of each item he is having, and we quickly have a total of the carbs he will be eating for that meal. This approach will save you alot of time and will allow you to more easily get other caregivers (your mother, in-laws, babysitters etc.) more comfortable with doing the calculations of counting carbs. It will put your mind at rest as well knowing that other caregivers are more likely to get it right if they use your tool you set up in advance. If you want an example, just send us a note and we can send you a copy of our spreadsheet. If you are not comfortable with excel or do not want to get too technical by setting up a laptop in your kitchen, then getting a dedicated notebook to hold all the information is well worth the time to at least have the right information handy to do your calculations.
four cookies, and never a number that is divisible by three. If the Serving Size was two, he will then of course, want three. Given that, it is important to have a list of how many carbs is in one cookie. We set up an excel spreadsheet that we keep on a laptop in our kitchen. We have a tab for every meal that has all the things listed that he typically eats, and how many carbs are in the easily definable quantity that makes sense to use on a daily basis. We use weight for things like fruit and other things that are easily weighed, cookies and easily countable items, we keep on a per item basis. We then set it up so that all we have to do is enter the number of units or the weight of each item he is having, and we quickly have a total of the carbs he will be eating for that meal. This approach will save you alot of time and will allow you to more easily get other caregivers (your mother, in-laws, babysitters etc.) more comfortable with doing the calculations of counting carbs. It will put your mind at rest as well knowing that other caregivers are more likely to get it right if they use your tool you set up in advance. If you want an example, just send us a note and we can send you a copy of our spreadsheet. If you are not comfortable with excel or do not want to get too technical by setting up a laptop in your kitchen, then getting a dedicated notebook to hold all the information is well worth the time to at least have the right information handy to do your calculations.
Step 3: Set up Tools and Systems
As mentioned above, I highly recommend setting up a laptop or computer in a central area, preferably your kitchen. It doesn’t have to be a computer that will be able to multitask or manage gigabytes of data, even a $300 net book will do fine. Load it up with Microsoft Office so you can use Excel which will be a lifesaver once you set things up. If computers are not the thing for you, then try and set up an area with your calculator and notebook that will have all the information you collected about the carb value of each food your child eats separated out by meal. This will help not only you be organized, but it will make others more comfortable in doing the math and administering the right doses.
If you are using a pump, then a lot of the math will be done for you in the unit. That doesn’t mean that you won’t want the tools to be able to easily calculate how many carbs are going in their mouth for every meal.
We also tracked our child’s glucose levels every time we took a reading, as well as how many carbs. We also made notes at each dosage or reading about whether there were any other factors that may impact his levels, i.e. whether he was exercising, active, sick etc. We went heavy into tracking data in the beginning, but we found that it helped us understand our child’s rhythms better and made us ultimately be better at communicating with our doctors.
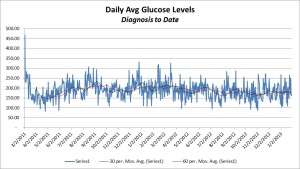
If you are using a pump, then a lot of the pump units will keep track of a lot of this for you (i.e. if you use the pump unit as the glucose meter such as with the omnipod). There are numerous apps, tracking software and websites that allow you to keep all this data in one place. We started off using an app and excel and found them to be our best solution. Everyone will have their own, but tracking the data will definitely help you get a hold of what is going on. See the chart below for a graph of every glucose reading we took for our child in the first couple of years. The first 550 reading was his reading when we brought him into the hospital when he was diagnosed.
Step 4: Teach Others Early – Share the Tools
When we first came home from the hospital, we were a bit overwhelmed about how we were going to go through the daily regimen that had been described to us by our doctors (7-12 finger pricks a day, counting carbs, doing all the math every time he ate, administering the insulin etc.). After the first couple of weeks, of we had our feet underneath us and started to get into a rhythm. Setting up all the tools as described above helped a lot. It was now time to make sure that we spread the knowledge about carbs, carb ratios, glucose meters, testing, the insulin pen etc. etc. etc. out to our babysitters grandparents and nurses at school. We worked hard to get them as familiar with what we were doing regarding his care as quickly as we could so they could ultimately be a backup and even give us a break to go out to dinner or a movie. Setting up the tools and writing out detailed instructions to which your “alternative caregivers” can refer is key. Also making sure that you have open lines of communication (i.e. our babysitter and school nurses typically text us our kid’s numbers) . Our babysitter, nurses etc. are now pros and that not only gives us peace of mind when we are away or when he is at school, but he is getting better day to day care which will keep his A1C levels (the 30 day average of his glucose levels) in line with his targets.
Step 5: Get out of the House – Take a Break
One thing that we learned in the early days was that it was important to keep perspective and to take a break from the hour to hour, day to day caring for your kid with his diabetes. Getting others involved in your child’s care early as described above is critical so that you can take some time for yourself. Dealing with any medical situation with a child is stressful, so it is important to remember that if you have a spouse, you are a team and need to spend some time together in the early days away from your care giving roles. That can involve getting out together as well as giving each other a break by telling your spouse to get out of the house for some time to themselves. If you are a single parent, then it will be equally as important to find some time to step away and get some time for yourself. If you have another child, like we do, it is also critical to make sure you spend some quality alone time with your non diabetic child. All of the attention on your child with diabetes can be quite daunting on the sibling. Our older boy is incredibly supportive and he is a wonderful big brother. We did have to make sure however, that no matter how “big” a kid we asked him to be in terms of being supportive, he is still a kid and we found it important to make him feel as special as he is.
Getting out of the house is also important as a family. Given how daunting all the math is etc., it can seem a bit easier to just stay home with the comfort of a food scale and the tools you have set up to calculate insulin doses. Life unfortunately is not always going to be in your kitchen, so we found that going out to lunch or dinner as a family forced us to figure out how to live with diabetes on the fly. Most restaurants have nutritional charts that will show the carbs, or you can find a lot of information on most chain restaurants on Calorie King. If not, then welcome to the “Art” part of diabetes care vs. the science. It as important to get good at estimating carbs in something that was made in a random diner. Our boy has a big appetite, so trying to figure out the carbs in some over sized pile of diner made french toast, eggs, bacon and whipped cream on top is always fun. You do the best you can, and you get better at it, but that will never happen if you stay in the house for sure.
Additional Note: Glucose Levels – What to Expect
Everyone is different and no two kids will follow the same path nor will they have the same reaction to insulin on a daily basis. Following is a chart for the first two years of our boy’s blood glucose readings. We are sharing this mainly to show that volatility is often the norm, but you get better at monitoring and keeping the highs down over time.
Our kid’s A1C started high and we have been able to get it down to around 7% on a pretty consistent basis. Every season brings new challenges. Summer is highly active and less scheduled vs. school months that are highly regimented with meal times at the same time every day. All those types of changes while his body is growing and changing daily.
We hope that you find some of the information above helpful!